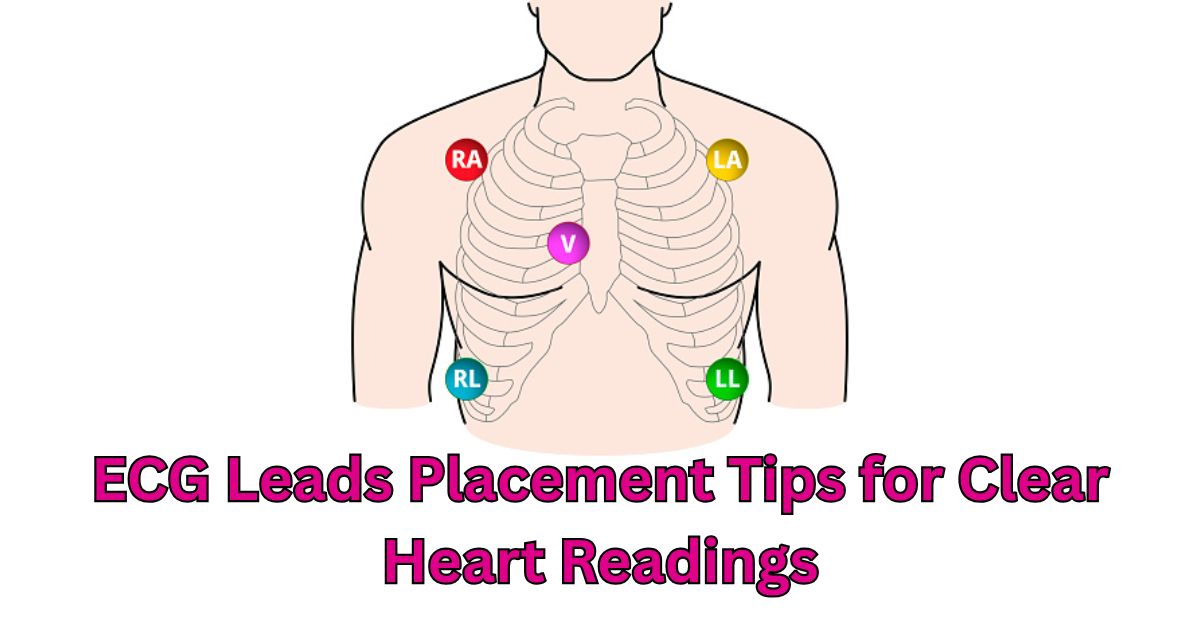
Placing the tiny sticky patches known as electrodes on the correct areas of your chest, arms, and legs follows ECG leads placement. From your heart, these patches gather signals and forward them to a machine, creating a cardiac trace. This is used by doctors to assess your cardiac performance.
Leads placed in the incorrect position can produce erroneous readings. That’s like peering through a foggy lens, you might overlook a major heart issue. Correcting it speeds up the diagnosis of heart disorders, including rhythm problems and heart attacks.
Among the several ECG configurations available are those with three leads, five leads, and twelve leads. Everybody adds varying degrees of detail.
Understanding ECG Leads and Their Functions
ECG leads placement is the deliberate arrangement of electrodes on the body to track heart electrical activity. These electrodes pick out electrical signals from the heart and send them to an ECG machine, which generates an electrocardiogram, a graphical depiction. Correct placement guarantees correct readings, which helps identify certain heart diseases.
Each of the several ECG systems has particular diagnostic uses. Basic monitoring and display of leads I, II, and III often use the 3 electrode approach. The 5 electrode method adds a chest lead to offer more exact information. Using 10 electrodes to capture a whole range of cardiac activity including limb and chest leads, the 12 lead ECG provides thorough heart examination.
You May Also Read This Blog: Different Types of Phototherapy Lights Available in Pakistan
Explanation of Limb Leads and Precordial Leads (V1–V6)
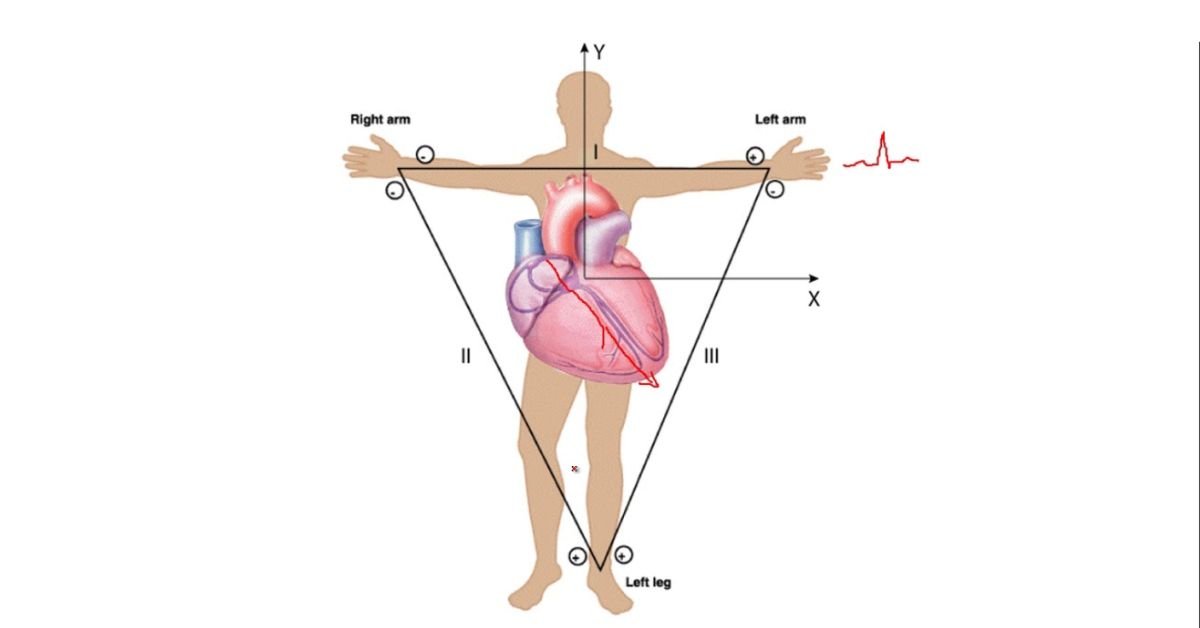
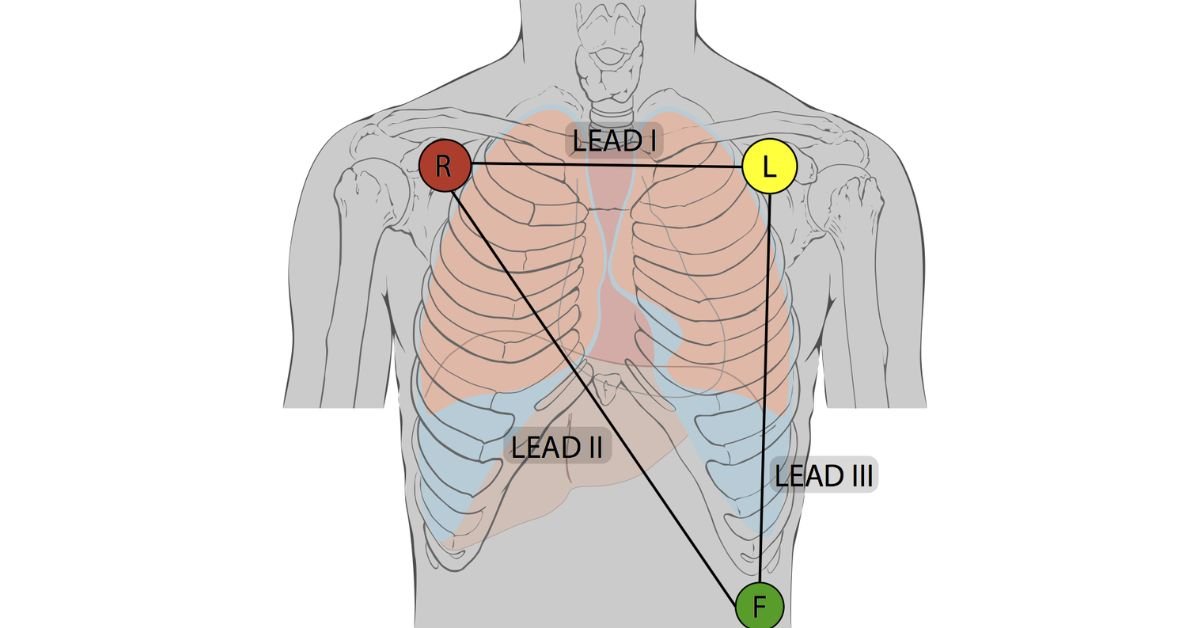
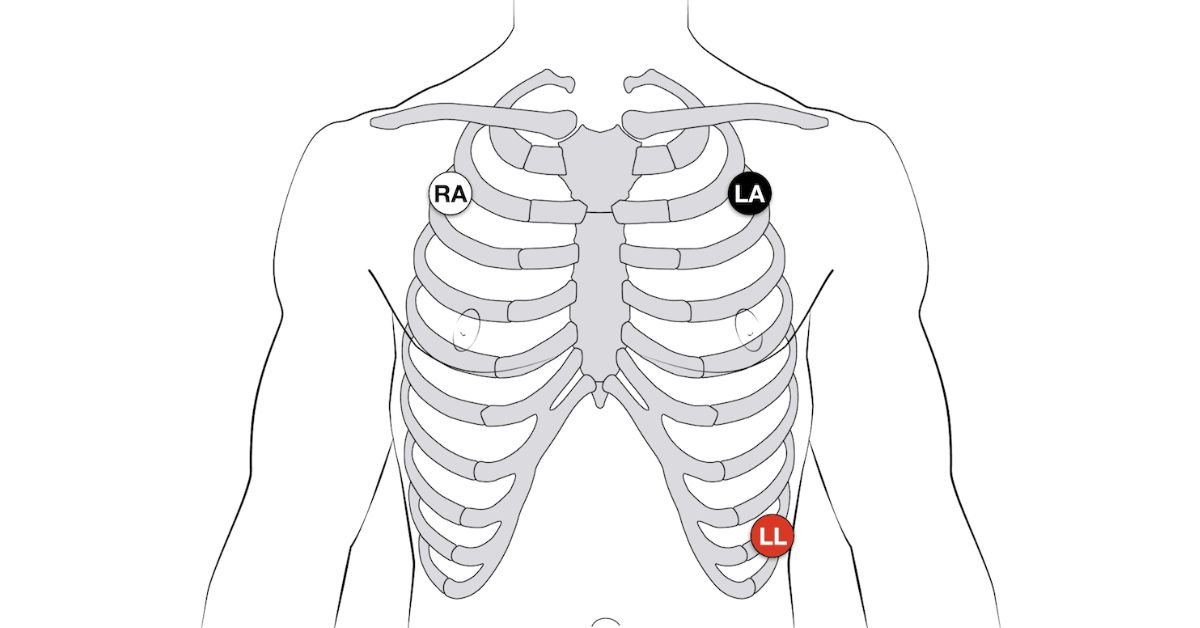
ECG leads placement begins with the limb leads, which include bipolar leads (I, II, III) and augmented limb leads (aVR, aVL, aVF). These are attached to the RA, LA, RL, and LL as part of the electrocardiogram setup. Together, they form Einthoven’s triangle, which helps the ECG machine view the heart from six angles. This view is essential for basic ECG interpretation and limb lead placement in any test.
Each limb lead plays a different role. Lead I measures left right signals, Lead II shows top to bottom, and Lead III focuses on the left leg. The augmented limb leads help improve signal strength. These leads are key in spotting signs of inferior STEMI and help compare results in a 3 lead vs. 5 lead vs. 12 lead ECG. These also support findings related to atrial flutter ECG patterns and AV dissociation in ventricular tachycardia.
Precordial Leads: V1–V6
The precordial leads (V1–V6) are chest leads that give a detailed view of the heart’s front and side. They follow the ECG electrode positioning guide and are placed on the chest using precordial lead landmarks. These include the sternum borders, intercostal space (ICS) landmarks, and midclavicular line placement. These are part of the 12 lead ECG placement, giving a full view of the heart’s chambers and wall motion.
Knowing how to place V1–V6 electrodes correctly helps doctors spot problems like right ventricular infarction (RV MI) or posterior myocardial infarction. V4R lead position for right ventricular infarction is used in right sided ECG (V4R), while posterior ECG leads for STEMI detection include posterior leads (V7–V9). The precordial leads also help detect rare signs like epsilon waves, support Fontaine lead setup for epsilon waves, and improve Lewis lead method to identify P waves in atrial flutter detection.
| Lead Group | Leads Included | Purpose |
| Limb Leads | I, II, III, aVR, aVL, aVF | Heart’s electrical activity from different angles |
| Precordial Leads | V1–V6 | Chest view of heart’s front, septum, and side wall |
This clear cardiac monitoring leads arrangement ensures precise results and supports proper diagnosis in clinical settings across Pakistan.
Einthoven’s Triangle and Its Significance
Einthoven’s triangle is made by placing bipolar leads (I, II, III) on the RA, LA, and LL using the correct ECG lead placement. These leads form a triangle that records the heart’s electrical signals from three angles. This setup is used in the 3 electrode system, 5 electrode system, and the full 12 lead ECG, making it the base of every electrocardiogram setup in hospitals and clinics across Pakistan.
This triangle is key in early heart check ups. It helps find rhythm problems and detect heart attacks like inferior STEMI. When placed right using the ECG electrode placement guide, it also improves the reading of augmented limb leads (aVR, aVL, aVF). These leads are needed for proper limb lead placement, and they support the comparison between bipolar vs. unipolar leads in advanced tests. This method supports cardiac monitoring leads in all types of patient cases.
| Lead | Position | View of Heart |
| Lead I | Right arm to left arm | Lateral side |
| Lead II | Right arm to left leg | Inferior side |
| Lead III | Left arm to left leg | Inferior lateral angle |
This triangle helps improve ECG interpretation, and works with chest leads like precordial leads (V1–V6). That’s why it’s important in both basic and advanced ECGs like Fontaine leads in ARVC, Lewis lead vs. standard lead for atrial activity, and in spotting ECG changes in atrial flutter or epsilon wave detection.
Frontal vs. Horizontal Plane Leads
Frontal plane leads come from the limb lead placement and show the heart’s electrical activity from top to bottom. These leads include bipolar leads (I, II, III) and augmented limb leads (aVR, aVL, aVF). This setup forms Einthoven’s triangle, which helps in spotting rhythm changes and conditions like inferior STEMI. These leads are part of every 12 lead ECG and are used in both 3 electrode and 5 electrode systems.
Horizontal plane leads are also called precordial leads (V1–V6) and focus on the heart’s front and side views. Proper ECG leads placement using precordial lead landmarks and ICS landmarks is key for clear results. These chest leads help in detecting right ventricular infarction (RV MI) and posterior myocardial infarction. Correct electrode positioning with these leads supports ECG interpretation, especially in Pakistan where fast and accurate diagnosis saves lives.
Step by Step Guide to ECG Leads Placement
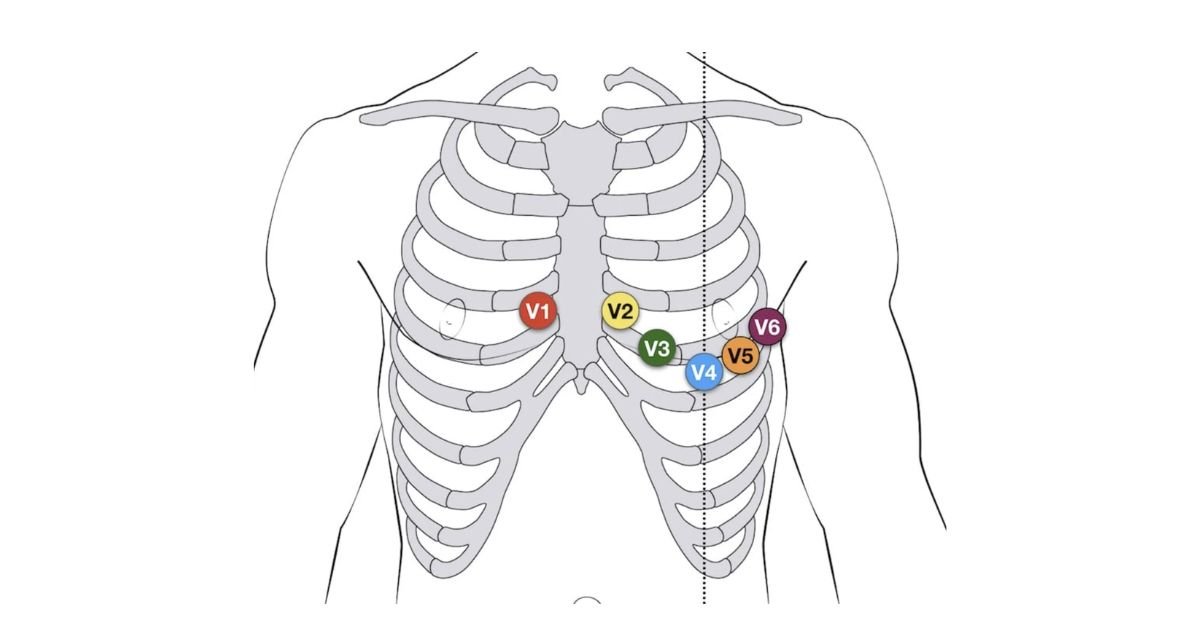
Proper ECG leads placement starts with clean skin and correct electrode positioning. The limb leads (RA, LA, RL, LL) go on the arms and legs, while chest leads or precordial leads (V1–V6) are placed using ICS landmarks, midclavicular line placement, and sternum borders. For the 12 lead ECG placement, each lead must follow the ECG electrode positioning guide to avoid errors in ECG interpretation.
How should one arrange V1–V6 electrodes? Start at the right fourth intercostal space for V1 and then keep across the chest until V6, close to the anterior axillary line. Basic cardiac monitoring leads are built from the 3 electrode system, the 5 electrode system offers greater detail. With a 12 lead ECG comprising bipolar leads (I, II, III), augmented limb leads (aVR, aVL, aVF), and precordial lead landmarks, full diagnosis detects inferior STEMI, right ventricular infarction (RV MI), and more.
Preparing the Patient and Equipment
Good patient preparation forms the foundation of correct ECG leads placement. The patient has to lie down calmly and with dry, clean skin. Better electrode location results from shaving chest hair and removing sweat. Particularly with a 12 lead ECG, this stage is crucial for accurate readings. Whether employing a 3 electrode system, 5 electrode system, or 12 lead ECG installation, good preparation also enhances the quality of cardiac monitoring leads.
All equipment should be checked before beginning the electrocardiogram setup. The ECG machine must be working, and all wires should be untangled and clean. The electrodes are placed according to the ECG electrode placement guide, ensuring they match precordial lead landmarks, sternum borders, and intercostal space (ICS) landmarks. Proper setup ensures that the limb lead placement and chest leads show clear waves for identifying inferior STEMI, atrial flutter detection, and epsilon wave detection.
Patient Positioning
For accurate ECG leads placement, the patient must lie in a supine, flat position on the bed. The body should be relaxed, and the limbs uncrossed. This keeps muscle activity low and avoids signal distortion. Correct posture is very important in ECG electrode placement, especially during a 12 lead ECG where clear heart signals help detect inferior STEMI or atrial flutter ECG patterns.
A calm and stable posture supports better readings from bipolar leads (I, II, III) and augmented limb leads (aVR, aVL, aVF). It also improves the accuracy of precordial leads (V1–V6) by aligning with the intercostal space (ICS) landmarks and midclavicular line placement. For special setups like Fontaine leads for arrhythmogenic RV cardiomyopathy or Lewis lead method to identify P waves, patient stillness is critical. This helps with precise electrode positioning and perfect signal pickup.
Skin Preparation
Good skin preparation is very important for accurate ECG leads placement. The skin should be cleaned with alcohol swabs to remove dirt and oil. If the chest is hairy, shaving may be needed to help the electrodes stick better. Clean, dry skin improves signal quality in both 3 electrode system and 12 lead ECG, especially when placing precordial leads (V1–V6) and limb leads (RA, LA, RL, LL).
Dry skin avoids interference in cardiac monitoring leads and ensures proper contact for chest leads, including posterior leads (V7–V9) and right sided ECG (V4R). This step also supports better outcomes in detecting inferior STEMI, atrial flutter ECG patterns, and right ventricular infarction (RV MI). Proper skin care is needed before using Lewis lead setup for P wave visibility and Fontaine lead setup for epsilon waves. Follow an ECG electrode positioning guide for best results.
Choosing the Right Electrodes
The success of ECG leads placement depends on choosing the right type of electrodes. Gel based electrodes help with better electrical contact and signal clarity in cardiac monitoring leads. Strong adhesive quality is also important so the electrodes stay in place during a 12 lead ECG, especially when placing precordial leads (V1–V6) and limb leads (RA, LA, RL, LL) during patient movement or sweating.
High quality electrodes improve accuracy for atrial flutter detection, epsilon wave detection, and ECG changes in atrial flutter. The use of proper electrodes is very important in detecting posterior myocardial infarction, inferior STEMI, and right ventricular infarction (RV MI). For advanced setups like Lewis lead setup for P wave visibility or Fontaine leads for arrhythmogenic RV cardiomyopathy, the right electrodes also improve ECG interpretation and reliability of ECG electrode positioning guide in all types including 3 electrode system, 5 electrode system, and full 12 lead ECG placement.
Limb Leads Placement (Standard 12 Lead ECG)
In ECG leads placement, proper limb lead placement is rather crucial. Four electrodes RA (right arm), LA (left arm), RL (right leg), and LL (left leg) are put on the limbs in a 12 lead ECG. For precise cardiac monitoring, these leads help create Einthoven’s triangle, which records the bipolar leads (I, II, III) and augmented limb leads (aVR, aVL, aVF).
Proper ECG electrode positioning guide ensures stable signals during electrocardiogram setup. These leads detect atrial flutter ECG patterns, changes from inferior STEMI, and help in atrial flutter detection. Difference between bipolar and unipolar leads must be understood for correct ECG interpretation. In 3 lead vs. 5 lead vs. 12 lead ECG, only the 12 lead ECG placement gives complete limb and chest leads data for accurate results in cases like right ventricular infarction (RV MI) or posterior myocardial infarction.
RA (Right Arm)
Standard ECG leads placement places the RA (right arm) electrode either on the upper arm or the right wrist. In a 12 lead ECG, this is component of the limb lead location. Correct electrode placement is crucial since enhanced limb leads aVR and the RA lead record the electrical signals of the heart in bipolar leads I and II.
For disorders like right ventricular infarction (RV MI), particularly, this lead promotes accurate ECG interpretation. Part of Einthoven’s triangle, the RA electrode detects AV dissociation in ventricular tachycardia, inferior STEMI, and atrial flutter ECG patterns. Stable contact at the wrist guarantees improved tracing for all kinds of cardiac monitoring leads, including a 3 electrode system, 5 electrode system, or complete 12 lead ECG installation, according to the ECG electrode location guidance.
LA (Left Arm)
Depending on patient comfort and skin condition, the LA (left arm) electrode attaches to the left wrist or upper arm in ECG leads placement. Essential for full 12 lead ECG accuracy in an electrocardiogram setup, this posture helps to record bipolar leads I and III as well as augmented limb lead aVL.
Good limb lead placement guarantees excellent cardiac monitoring leads for ECG interpretation. One angle of Einthoven’s triangle formed by the LA electrode aids in the detection of conditions like atrial flutter ECG patterns, right ventricular infarction (RV MI), and inferior STEMI. Here stable electrode placement covers all systems including 3 electrode system, 5 electrode system, and complete ECG electrode placement guidance, so boosting visibility of epsilon wave detection and AV dissociation in ventricular tachycardia.
RL (Right Leg)
Attached to the right ankle or lower leg, the RL (right leg) electrode of ECG leads placement. This records not only electrical signals. It is the ground electrode used during ECG interpretation to assist in the reduction of noise and a clear signal promotion. This guarantees correct readings in all ECG systems including the whole 12 lead ECG, 3 electrode, and 5 electrode systems.
By finishing the ECG configuration, the RL lead significantly helps to stabilize cardiac monitoring leads. The ECG electrode positioning guide would not function as it should without this grounding. It helps better detection of epsilon wave, atrial flutter ECG patterns, and AV dissociation in ventricular tachycardia even though it does not influence bipolar leads like I, II, and III or unipolar leads like aVR. For 12 lead systems, this is therefore crucial for any proper ECG electrode placement.
LL (Left Leg)
The LL (left leg) electrode in ECG leads placement hooks to the left ankle or lower leg. Completing Einthoven’s triangle depends on this lead, which also forms part of the four limb leads used in a 12 lead ECG. For proper ECG interpretation in both hospitals and field configurations, the LL lead aids in creating bipolar leads I, II, III and augmented limb leads (aVR, aVL, aVF).
Complete ECG setup for the detection of cardiac diseases including right ventricular infarction (RV MI) is supported by this electrode placement. Correct limb lead placement lets doctors clearly examine electrical activity under 3 electrode system, 5 electrode system, or full 12 electrode ECG implantation. Especially when used with Lewis lead and Fontaine leads for advanced monitoring, correct use also helps to identify atrial flutter ECG patterns, AV dissociation in ventricular tachycardia, and epsilon wave detection.
Importance of Symmetry and Avoiding Bony Prominences
Using symmetry guarantees correct and obvious findings in ECG leads placement. To prevent signal problems, the limb lead location must be equal on both sides of the body. Particularly in a 12 lead ECG configuration, good electrode placement enables appropriate measurements of bipolar against unipolar leads. It also supports the diagnosis of heart diseases like posterior myocardial infarction without misunderstanding or misleading alterations and right ventricular infarction (RV MI).
In ECG setup, another crucial avoidance is from bony prominences such as elbows, wrists, and collarbones. These regions can produce noise in signals by interfering with skin contact. Placing electrodes on soft, flat surfaces increases contact and aids in AV dissociation in ventricular tachycardia, epsilon wave detection, and atrial flutter detection. Correct ECG electrode placement for 12 lead systems must follow the ECG electrode positioning guide, considering ICS landmarks, sternum borders, and precordial lead landmarks, therefore ensuring reliable ECG reading.
Precordial (Chest) Leads Placement (V1-V6)
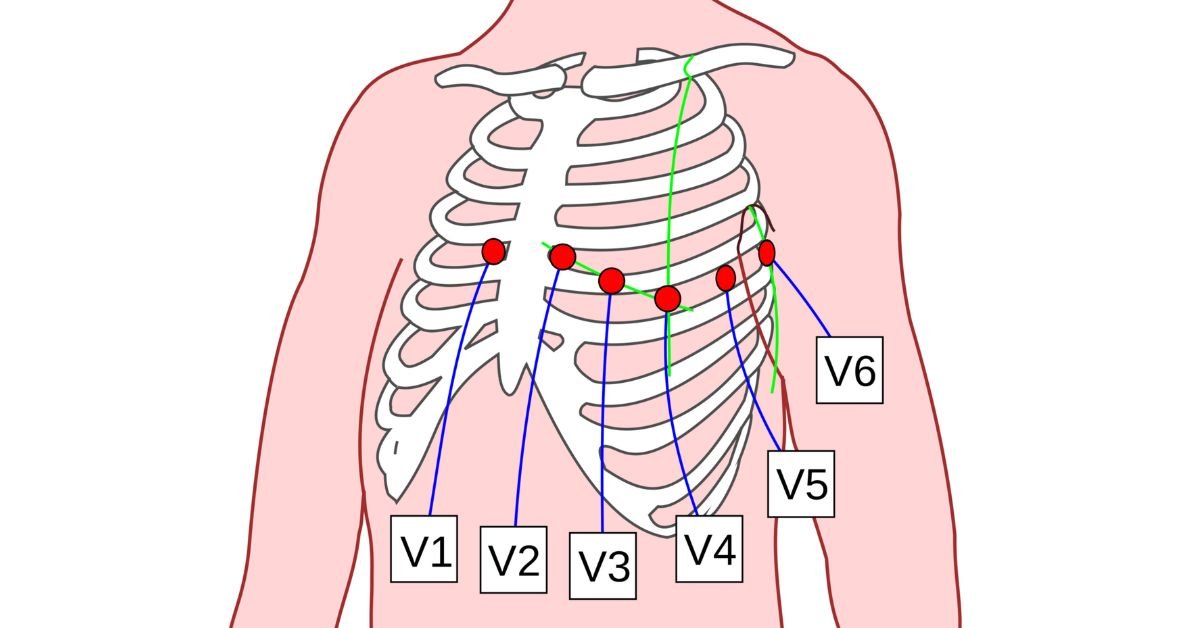
The precordial leads (V1–V6) put on the chest in ECG leads placement provide a clear image of the electrical signals of the heart. These leads comprise the 12 lead ECG, hence proper electrode placement is rather crucial. In the 4th intercostal space (ICS), V1 and V2 span each side of the sternum. V4 crosses the midclavicular line and V6 crosses the anterior axillary line.
Every chest lead reveals activity in many areas of the heart. This aids in the detection by doctors of disorders such as atrial flutter ECG patterns, right ventricular infarction (RV MI), and inferior STEMI. Exact precordial lead landmarks let professionals prevent mistakes by using the ECG electrode placement guidance. Early ECG interpretation, epsilon wave detection, and AV dissociation in ventricular tachycardia are all benefited from correct ECG electrode placement for 12 lead ECG.
V1
The V1 lead in ECG leads placement crosses the sternum on the right side at the 4th intercostal space (ICS). This location records signals coming from the right ventricle. Correct V1 electrode placement is essential to identify major problems including ECG leads for inferior STEMI and right ventricular infarction (RV MI). Under a 12 lead ECG system, this lead falls among the precordial leads (V1–V6).
Especially for atrial flutter diagnosis and epsilon wave detection in Fontaine leads for arrhythmogenic RV cardiomyopathy, the V1 lead aids in early ECG interpretation. The electrode placement landmarks have to follow the ECG electrode placement guidance, the chest needs to be dry and clean. When done right, bipolar against unipolar leads disparities become more evident. Whether in a 3 electrode system or a 5 electrode system, this enhances the outcomes of cardiac monitoring leads, particularly in the healthcare environment all throughout Pakistan.
V2
The V2 lead is positioned in ECG leads placement at the left sternal border at the fourth intercostal space (ICS). It provides an unambiguous perspective on the front of the heart. In the 12 lead ECG, this posture is part of the precordial leads (V1–V6) and enables clinicians to identify heart disorders such as inferior STEMI and right ventricular infarction (RV MI).
To observe atrial flutter ECG patterns and epsilon wave detection, proper electrode placement of V2 is crucial in ECG interpretation. The V2 lead sits exactly across from V1 following the ECG electrode location instructions, so becoming part of the proper ECG chest lead architecture. Whether in 3 electrode system, 5 electrode system, or 12 lead ECG placement, strict adherence to the intercostal space (ICS), sternum borders, and precordial lead landmarks helps to avoid mistakes in cardiac monitoring leads.
V3
The V3 electrode in ECG leads placement is perfectly straight line between V2 and V4. In the 12 lead ECG system, which provides a whole view of the heart, this posture is crucial. Especially in situations of inferior STEMI and right ventricular infarction (RV MI), appropriate ECG electrode placement of V3 enables doctors to clearly observe the front wall of the left ventricle.
Correct intercostal space (ICS) landmarks and aligned with the midclavicular line placement help the precordial leads (V1–V6) be put. V3 helps with better ECG interpretation by connecting impulses between the right and left sides of the chest. One should grasp the differences between bipolar and unipolar leads during setup. Particularly with 12 lead ECG placement as opposed to 3 lead vs. 5 lead systems, following the ECG electrode placement instructions guarantees precise cardiac monitoring leads.
V4
The V4 electrode is placed in ECG leads at the 5th intercostal space, oriented with the midclavicular line. Accurate depiction of the electrical activity of the heart depends on its positioning. It facilitates the diagnosis of disorders including inferior STEMI and posterior myocardial infarction. Correct placement of the lead by the ECG electrode positioning guide guarantees the general quality of the ECG is improved.
Part of the precordial leads (V1–V6) used in a 12 lead ECG is the V4 lead positioning. It offers an excellent picture of the left ventricle, therefore contributing to complete heart monitoring. Accurate ECG interpretation depends on correct chest leading posture. Bad electrode placement could produce false findings. For any healthcare practitioner, thus, knowledge of the intercostal space (ICS) landmarks and midclavicular line location is indispensable.
V5
The V5 electrode should be positioned on the anterior axillary line yet maintained at the same level as V4 for ECG leads placement. Evaluating the left ventricle’s lateral wall depends on this positioning. Correct positioning aids in the identification of disorders including right ventricular infarction (RV MI) and inferior STEMI. Precise lead placement depends on the ECG electrode location guidance.
A clean 12 lead ECG is obtained in great part from the V5 lead, which is part of the precordial leads (V1–V6). It is required for the interpretation of ECGs and offers vital data on the electrical activity of the heart. Correct electrode placement improves the accuracy in identifying anomalies including atrial flutter and Epsilon waves. Precise chest lead placement guarantees consistent cardiac monitoring.
V6
The V6 electrode should be positioned in ECG leads placement same like V4 but along the midaxillary line. Clear readings from the cardiac lateral wall depend on this posture. Correct placement of precordial leads (V1–V6) guarantees correct readings in 12 lead ECG and helps detect problems such as posterior myocardial infarction or right ventricular infarction (RV MI).
Precise cardiac monitoring depends on correct placement of the ECG electrodes. Found at the midaxillary line, the V6 lead greatly influences ECG interpretation. It helps to better identify heart disorders including atrial flutter detection and inferior STEMI. Precise alignment of chest leads such as V6 enables improved ECG electrode positioning compliance, therefore guaranteeing a clear and consistent reading.
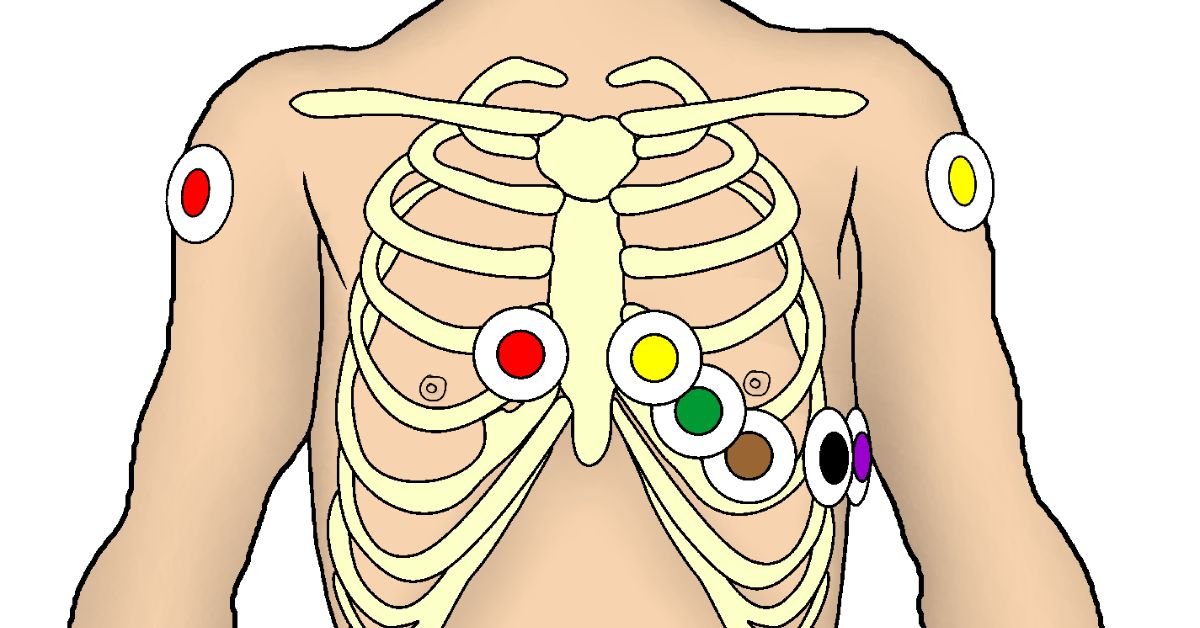
Visual diagram reference for accuracy
In ECG leads installation, exact electrode placement depends on visual diagram use. Particularly in intricate configurations like the 12 lead ECG, this visual reference enables medical practitioners to precisely insert electrodes. Correct ECG electrode placement reduces the possibility of misinterpretation, allowing the diagnosis of disorders like posterior myocardial infarction (RV MI) and right ventricular infarction.
A visual diagram guides the precordial leads (V1–V6) and their precise positions on the chest. It also improves the whole ECG electrode positioning guide by helping to correct the location of limb leads (RA, LA, RL, LL) and chest leads. Clear and consistent readings which are essential for the diagnosis of heart diseases including inferior STEMI or atrial flutter detection are guaranteed by appropriate positioning.
Special Lead Placements (Additional Configurations)
Under some clinical circumstances, ECG leads placement calls for unique lead configurations outside the conventional 12 lead ECG. Right sided ECG, for instance, (like V4R for right ventricular infarction) entails shifting precordial leads to track the right side of the heart. Furthermore, posterior myocardial infarction which might not be obvious in a conventional 12 lead ECG can be found using posterior leads (V7–V9).
Accurate ECG interpretation in circumstances such as inferior STEMI or atrial flutter identification depends on these particular lead locations. Furthermore improving the visibility of epsilon waves and P waves correspondingly are special setups including Fontaine leads or Lewis leads. Correct placement of ECG electrodes in the diagnosis of complicated heart diseases depends on an awareness of these particular locations.
Right sided ECG (V1R-V6R)
Special ECG lead placement used to evaluate right cardiac problems is right sided ECG (V1R–V6R). It is primarily used in cases of suspected right side of the heart cardiac disorders including various conditions or right ventricular infarction (RV MI). Particularly with V4R, the positioning of precordial leads (V1–V6) on the right side of the chest facilitates correct monitoring and diagnosis of these disorders.
This arrangement is absolutely essential for spotting alterations in right ventricular infarction that might not be seen on a conventional 12 lead ECG. It aids in assessing disorders including inferior STEMI and atrial flutter detection as well. For right sided precordial leads and cardiac monitoring leads, appropriate ECG electrode placement in the right chest area offers a sharper image of the heart’s electrical activity, therefore guiding doctors’ diagnosis judgements.
Posterior Leads (V7-V9)
The ECG lead placement must include posterior leads (V7–V9) if one is to detect posterior myocardial infarction (MI). These leads are positioned on the rear of the chest to offer a better perspective of the posterior wall’s electrical activity of the heart. With precordial leads (V7–V9), doctors can more effectively identify ECG alterations suggesting a posterior MI, which can be challenging using conventional 12 lead ECG.
Given a suspected inferior STEMI, using posterior leads is very crucial. Doctors can track the posterior wall activity of the heart by means of the ECG electrode implantation at certain intercostal space (ICS). This ECG electrode placement guidance guarantees correct diagnosis of posterior myocardial infarction, so enabling doctors to act in the required direction for efficient therapy and care.
Lewis Lead (S5 Lead)
Monitoring atrial activity in ECG lead placement is much aided by the Lewis lead (S5 lead). Crucially important for the diagnosis of atrial flutter and other atrial arrhythmias, it aids in P wave detection. In the 3 electrode system, proper electrode placement guarantees that the Lewis lead offers a clear view of the cardiac electric activity. Patients with atrial flutter detection sometimes use this lead arrangement in order to better grasp their heart rhythm.
Furthermore, the Lewis lead configuration facilitates more efficient monitoring of atrial activity than does conventional ECG leads. Placing the electrodes at particular precordial lead sites improves P wave visibility. This might help one understand the ECG interpretation of atrial flutter ECG patterns or identify anomalies in the atrial function. In advanced 12 lead ECG setups especially, the Lewis lead is quite useful.
Fontaine Leads
Fontaine leads are specific ECG leads placed in unusual circumstances such as arrhythmogenic right ventricular cardiomyopathy (ARVC). Their main ability to diagnose ARVC is to identify epsilon waves. These leads are positioned precisely to give a better picture of the electrical activity of the heart, particularly in cases when regular leads’ placement is challenging.
Accurate ECG interpretation in patients with some cardiac diseases depends on the Fontaine leads in clinical environments. Their electrode placement enables the capture of particular trends that conventional leads would overlook. They are a vital tool in specialised cardiac problems since they help to identify anomalies that could go undetectable in a regular 12 lead ECG system.
Common ECG Lead Placement Mistakes & How to Avoid Them
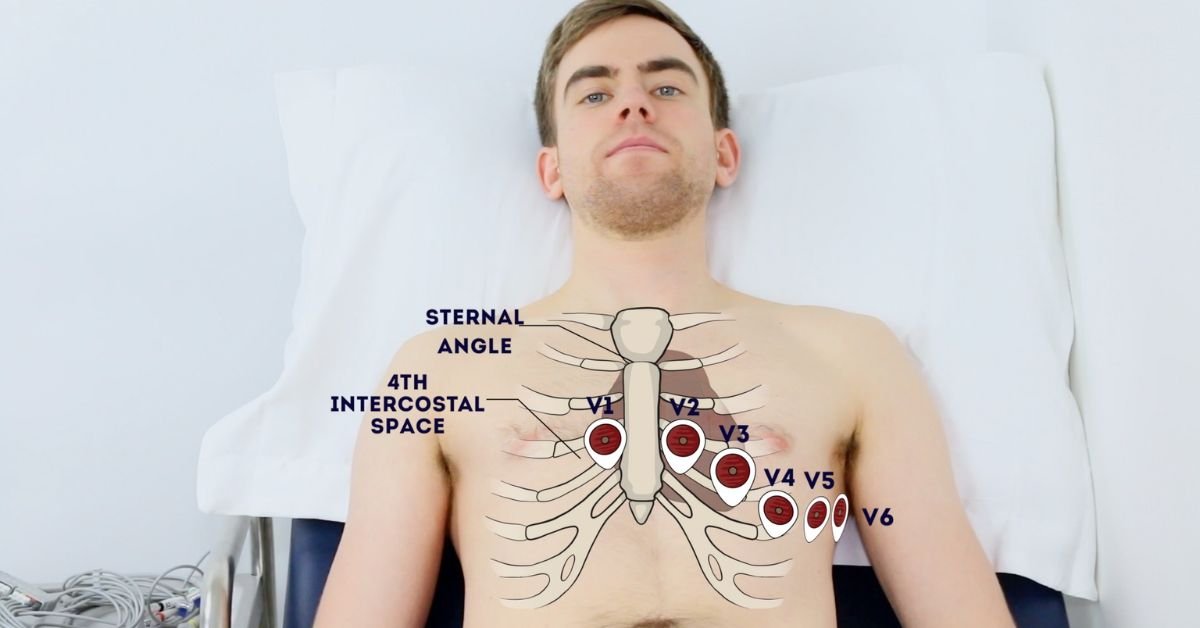
Correct heart monitoring depends on proper ECG lead placement. A common error is V1/V2 electrode placement either too high or too low. This misplacing can skew the readings and compromise the diagnosis. To prevent mistakes, make sure the V1/V2 leads land in the proper intercostal areas. Good posture will produce clear findings and enable correct ECG interpretation.
Another frequent problem is limb lead reversals that is, changing the RA/LA and RL/LL locations. Incorrect readings resulting from this can complicate diagnosis of heart disease. Furthermore causing artefacts are electrodes positioned over muscles or bony regions. Always correctly prepare the skin by cleansing the region and guaranteeing appropriate skin contact to avoid this. This guarantees exact ECG electrode placement and high quality readings.
Tips for Reducing Artifacts and Improving ECG Quality
Minimizing patient movement is quite vital to guarantee accurate results and optimise ECG lead placement. Patients moving during the test can produce artefacts distorting the readings. Patients should be reminded to still themselves throughout the ECG recording. Furthermore ensure that the electrodes adhere properly to the skin to prevent signal interference resulting from loose connections, therefore affecting the ECG interpretation.
Eliminating electrical interference is another essential action towards bettering ECG quality. Turning off surrounding equipment that might produce electrical signals will help to avoid ECG trace distortion. Always review the lead connections to guarantee they remain stable during extended ECG recordings as well. This guarantees that ECG electrode placement stays exact all during the operation, so offering the most dependable cardiac monitoring and lowering the possibility of artefacts in the final outputs.
Best Practices for ECG Lead Placement
Following standard colour coding is absolutely necessary for correct ECG lead placement. Clear instructions on electrode colours for appropriate identification come from the AHA and IEC standards. Double checking anatomical landmarks guarantees correct limb lead (RA, LA, RL, LL) and precordial lead (V1–V6) placement. These criteria help doctors lower the danger of misplacing, therefore improving the ECG interpretation and reliable cardiac monitoring.
Teaching patients about being motionless and calm during the operation is equally vital. Movement might produce artefacts or noise, therefore influencing the quality of the 12 lead ECG. Minimising mistakes also depends critically on employing premium electrodes and guaranteeing well maintained ECG devices. These techniques guarantee the positioning of the ECG electrode, so producing consistent ECG readings and improved patient results.
Conclusion
Getting accurate and consistent heart measurements depends on ECG leads placement. Correct electrode placement guarantees clear findings, so guiding medical practitioners in their selections. To prevent mistakes and raise diagnostic accuracy, always follow accepted norms for electrode placement. Recall, even little errors in ECG lead placement can produce erroneous findings. Always give accurate placement top priority for the greatest results in cardiac treatment, bookmark this guide for quick access.
FAQ’s
What is the best practice placement of ECG leads?
Following a consistent colour coding, verifying anatomical landmarks, and guaranteeing appropriate electrode adhesion for precise ECG lead insertion constitute the best practices.
How to remember where to put ECG leads?
Familiarise yourself with important anatomical features such as the sternum boundaries and intercostal spaces (ICS) using the AHA or IEC colour coding schemes.
How to get a perfect ECG?
For a clean ECG recording, guarantee correct ECG electrode insertion, prevent patient movement, and use premium electrodes and well maintained equipment.
What is the proper placement of cardiac leads?
Confirm correct skin contact for accurate results by placing the limb leads on the limbs, precordial leads (V1–V6) on the chest.
Where is the best 5 lead ECG placement?
For a 5 lead ECG, for best monitoring, position the limb leads (RA, LA, RL, LL) and two precordial leads (V1, V5) at the chest’s midline and left side.
How to check if an ECG report is normal?
Consistent P waves, QRS complexes, and T waves with regular cardiac rhythm and no notable anomalies present on a typical ECG report.