Have you ever wondered the reason your lab’s results aren’t working even though you’re certain you’ve followed each step? You wash your equipment and you prepare the samples but there’s not right. It’s frustrating, right? It was exactly the way I felt when first realized how important sterilization actually is. It turns out that if your equipment isn’t properly sterilized everything else you do won’t be of any use. That’s where the autoclave is needed.
In this article you’ll discover the basics of what an autoclave in microbiology does what it does, how it operates and how it can be an essential tool to keep your laboratory clear and accurate. The information will be explained in simple English and, even if you’re not familiar with this topic, you’ll be able to grasp the information quickly. In the end you’ll understand how autoclaves can prevent contamination, cut down on time, and ensure that your results are accurate and accurate. So, let’s get started. You’re at the right spot.
What Is an Autoclave?
An autoclave in microbiology can be described as steam sterilizers utilized to clean lab equipment, tools and waste. It utilizes the pressure of steam to eliminate microbes and contaminates, as well as destroy bacteria that are resistant to heat. This creates a clean and safe environments for hospitals and labs in Pakistan.
The autoclave machine operates within an enclosed pressure chamber. It is able to maintain high sterilization temperatures and pressure to ensure biological decontamination. It aids in the sterilization process of preparation of culture media instrumentation that can be reused, and also laboratory waste that is contaminated by the process of thermal disinfection as well as infection control.
Autoclave Principle/ Working
The principles behind steam sterilization rest on the generation of steam and the steam pressure that destroys any living microorganisms. The steam cycle heats up the chamber to a high temperature, allowing sterilization that allows the coagulation of proteins, the destruction of spores and the safely disposing of waste. This is crucial to the sterilization of healthcare.
The autoclave process begins by heating water to produce saturated steam. The steam is able to penetrate the materials within the chamber for sterilization. The indicators for sterilization confirm the process. This is a great way to understand understanding the significance of using autoclaves to ensure safe cleaning of medical equipment and safety in the laboratory.
How Does an Autoclave Work?
The working principle of an autoclave relies upon the elimination of air through the force of gravity, or by vacuum. Then, the sterilization using vacuum is completed by filling the chamber with steam that is high pressure. Steam kills bacteria and microorganisms by using humid warmth. Tools are then stored for a specific autoclave duration at a set temp and pressure.
The autoclave’s components comprise the safety valve for pressure as well as the whistle (pressure release) and pressure gauge and the vacuum pump. Autoclaves that are properly maintained require monitoring temperature and checking for leaks. This step is necessary to ensure sterility and autoclave maintenance for labs and hospitals.
You May Also Read This Blog: Phototherapy Machine: How It Works & Why Hospitals Use It
Principle and Working of Autoclave
Based on Capasee Electro Medical Engineering, their lab autoclave models have been designed with the latest pressure monitoring equipment. The systems they use support positive pressure displacement autoclaves as well as Autoclaves with gravity displacement models. They allow for full steam penetration as well as biohazard protection for all autoclavable substances.
Capasee utilizes wastewater cooling systems as well as vacuum generators to ensure secure disposal. The autoclave calibration is guaranteed to produce the same autoclave cycle results. These units help prevent healthcare associated infections (HAIs). The technique also permits application in disinfection of instruments as well as sterilization of waste and autoclaves in prevention of infections programs.
| Feature | Description |
| Steam Pressure | High pressure allows deeper steam penetration |
| Sterilization Temperature | Usually 121°C to 134°C |
| Sterilization Indicators | Show complete sterilization has occurred |
| Pressure Safety Valve Function | Prevents over pressure accidents |
| Vacuum Pump | Removes air for proper decontamination |
This is a brief but thorough explanation of the differences between moist and dry sterilization processes, and how autoclave helps prevent contamination in laboratories. You can autoclave items made of plastic when they’re marked as for autoclaving, and if you follow procedures for safety in the laboratory.
Components of Autoclave and Their Functions
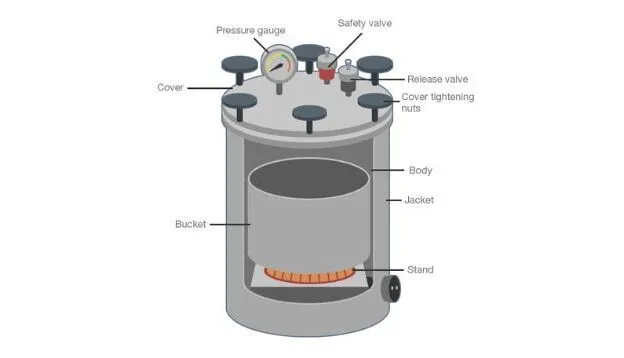
Autoclave in microbiology utilize the most important components of an autoclave such as the lid, pressure chamber the pressure gauge, the whistle (pressure release) and safety valve that performs the process of moist sterilization by heating. The pressure chamber houses the sterilization chamber in which items undergo steam treatment under pressure. This assists in the inactivation of microbial through the attainment of the correct temperatures and the right pressure to allow thermal sterilization as well as biological decontamination.
The lid of the chamber is sealed to keep steam pressure in check and prevent contamination. The pressure gauge monitors steam generated and ensures that the autoclave’s cycle is within the safe boundaries. The safety valve and the whistle restrict steam release to protect the user and the machine. The two components together provide sterilization and help with infection control in labs as well as hospitals for sterilization of medical waste and sterilization of instruments.
Pressure Chamber
Pressure chambers are the primary component of the autoclave machine. It houses the sterilization chamber, where things such as laboratory equipment and medical instruments are sterilized using thermal. The chamber must be able to withstand steam pressure and extreme heat in the autoclave cycle to ensure that microbial activity is completely eliminated. This is crucial to ensure sterility with steam under pressure to aid in biological removal of contaminants.
The pressure chamber is used in conjunction in conjunction with the vacuum pump eliminate air, which allows for better steam to penetrate. It helps keep the sterilization temperature as well as the pressure stable throughout the process of steam. A proper pressure monitoring system is essential for the control of infections and aids in the sterilization process of waste, specifically for lab waste that is contaminated in research and healthcare settings.
Lid / Door
A lid closes the chamber tight to keep the steam that is saturated within. It stops steam from leaving during the autoclave process. The lid is secured to ensure that the pressure of the steam sterilizer remains at a level that is sufficient to ensure sterility. This is essential to ensure safety and effectiveness in the use of autoclaves in laboratories and healthcare sterilization.
The door is usually locked automatically in operation to avoid injuries. It ensures safety for autoclaves by allowing the steam to be held inside the. The lid works closely with the pressure gauge and safety valve to maintain balance, supporting best practices in autoclaving and preventing healthcare associated infections (HAIs).
Pressure Gauge
The gauge of pressure displays the current steam pressure within the chamber of pressure. It assists users in monitoring the sterilization pressure to ensure that the autoclave has reached the ideal conditions. This instrument is crucial to ensure that the autoclave is operating according to its principle of killing microorganisms that resist heat by the process of moist heat sterilization.
Continuous monitoring of pressure enables the user to modify the process if required. The pressure gauge integrates in conjunction with the temperature monitoring system to ensure proper setting of sterilization temperatures as well as pressure. This helps to ensure safety protocols in the laboratory and also helps verify the autoclave cycle time to ensure the effective sterilization of instruments.
Pressure Releasing Unit / Whistle
The pressure releasing device is often referred to as the whistle, lets out excessive steam to ensure the safety of the chamber. It manages the pressure throughout the sterilization process of steam to ensure that accidents are not caused by excessive accumulation. The unit plays an essential part in the safety of autoclaves by regulating steam production and release.
If the pressure exceeds a certain limit, the whistle is triggered to alert the user. This feature is paired together with the safety valve to ensure balance and stop dangerous pressures. It helps ensure an efficient operation and helps to prevent injury to the autoclave and the sterilized material, ensuring the safety of medical waste sterilization.
Safety Valve
The safety valve guards the autoclave by releasing steam automatically in the event that pressure gets excessively. The valve functions as a backup for the pressure release unit and protects against dangers of explosions. It is an integral element of the autoclave process step by step to ensure that the pressure safety valve functions.
The valve makes sure that steam from high pressure remains within the safe limits, thereby assisting the prevention of infections along with thermal disinfection. Regular inspections and maintenance of the autoclave ensure that the safety valve functions correctly. This is essential to ensure the safety of labs and protecting equipment and users in Pakistan’s microbiology and healthcare laboratories.
Steam Generator, Vacuum Generator, and Wastewater Cooler in Autoclave in Microbiology
The steam generator, also known as an electrical heater is an essential part of an autoclave device. It produces saturated steam at a suitable temperature and pressure for sterilization. The steam sterilizer generates steam under pressure. This allows for efficient moist heat sterilization for sterilization of instruments as well as culture media sterilization. The steam generator supports the process of thermal sterilization as well as microbial inhibition to ensure a sterile atmosphere in hospitals and laboratories.
Vacuum generators, utilized in certain types of autoclaves, assists in the removal of air from the chamber of pressure. This improves steam penetration and accelerates the autoclave process. The wastewater cooler is able to cool hot water following sterilization. It plays an important role in biohazard prevention and the safe disposal of laboratory wastes that are contaminated. Together, these components provide the safety of labs, infection control as well as effective sterilization of medical equipment with a proper autoclave process and regular maintenance.
Read More: Our Products
Procedure for Running an Autoclave

The autoclave process begins with the placement of autoclavable items in the chamber for sterilization. The door needs to be securely shut to ensure an atmosphere of pressure. The steam production creates steam when water is heated under pressure, and reaches the proper temperatures and the pressure needed to eliminate bacteria that are resistant to heat. The autoclave is run for a predetermined period of period of time, allowing steam to penetrate to ensure the inactivation of microbial growth as well as thermal sterilization for laboratory equipment as well as medical instruments. A proper pressure and temperature monitoring provide the sterility of your equipment.
Following the cycle, steam is released safely via the pressure safety valve (or whistle) (pressure release). The autoclave cools off prior to opening. This helps in the prevention of infection and sterilization of medical waste. Autoclave safety precautions can prevent incidents, which makes this process suitable for medical and lab use. Noting the procedure on a sheet of a sterilization log is vital for the validation of autoclaves and to ensure that the biosafety standards are maintained.
How to Use an Autoclave
Utilizing the Capasee Electro Medical Engineering autoclave is based on the same fundamental steps for the autoclave’s working principle. To begin, you must charge the pressure cooker autoclave, or any other type of autoclave with autoclavable, clean materials. Turn on the steam sterilizer to begin the generation of steam. Set the sterilization temperature as well as pressure based on the type of material, generally around 121°C and 15psi. The duration of the autoclave cycle can vary, but it usually lasts between approximately 15 to 30 minutes.
This autoclave utilizes a vacuum assisted sterilization for improved steam penetration especially in wraps or dense instruments. Safety features such as that of the safety gauge as well as pressure gauge guarantee the safety of your operation. After sterilization, you must wait for the pressure to completely release prior to opening. This careful method guarantees instrument sterilization, culture media sterilization, and waste sterilization, promoting a sterile environment and preventing healthcare associated infections (HAIs). Regular maintenance and calibration of the autoclave keeps the machine running and efficient.
Types of Autoclave
Autoclaves in microbiology come in a variety of types, each specifically designed to meet specific sterilization requirements. The pressure cooker autoclave (N-Type) is small and perfect for small labs. It utilizes steam under pressure inside the pressure chamber to provide quick humid heat sterilization. It is ideal for sterilizing instruments and media sterilization.
A gravity displacement autoclave functions by pushing air out using large steam to ensure steam penetration. Positive pressure displacement autoclave (B-Type) is used to force heated steam through instruments to aid in microbiological inactivation. The autoclave that is negative pressure displacement (S-Type) removes air by using the vacuum pump prior to steam is pumped into the chamber. This kind of autoclave ensures complete biological decontamination, and is used in hospitals for sterilization of medical waste.
How to Choose the Right Type of Autoclave for Your Facility
The choice of the best autoclave is dependent on the needs of your. Smaller labs can benefit from bench based autoclaves for labs for hospitals, whereas hospitals require sophisticated models like the S-Type or B-Type for more thorough sterilization. Autoclaves all follow the autoclave process using high pressure steam for efficient thermal sterilization and security.
Capasee Electro Medical Engineering offers various models. The hinged autoclave with a single door works well for smaller labs, whereas the single door autoclave with vertical sliding fits moderate requirements. Double door pass thru autoclave and the dual chamber tower autoclaves are the best for hospitals with a lot of activity. They offer excellent sterility security Pressure monitoring, as well as adhere to strict safety guidelines for laboratories to reduce microbial contamination as well as keep the environment sterile.
Uses of Autoclave in Microbiology

The autoclave in microbiology plays an important role in the control of infections using high pressure steam in order to eliminate microbes that are resistant to heat. It aids in the sterilization of culture media instruments, sterilization of instruments, and sterilization of medical wastes through high temperature sterilization within the chamber for sterilization. The autoclave process step by process ensures that sterility is assured and stops microbial contamination from laboratories and in healthcare. The steam sterilizer operates through steam generation and penetration into an air pressure chamber. It destroys the spores and proteins by thermal sterilization.
Autoclaves can also assist in the decontamination of biological materials and secure handling of laboratory wastes that are contaminated. The autoclave process includes rigorous temperature monitoring and a the pressure safety valve to ensure that the temperature is completely disinfected. Utilizing a vacuum assisted sterilization method, air is removed that can block steam, thereby reduces the time it takes to complete an autoclave. This durable autoclave machine provides the sterility that is essential to the safety of healthcare facilities and for sterilization in laboratories in Pakistan’s hospitals and laboratories.
Precautions While Using Autoclaves
The use of an autoclave is a matter of taking careful autoclave security measures to avoid injuries. Always verify the gauge for pressure and the safety valve prior to beginning the autoclave process. Use the best practices for autoclaving to ensure safety steam sterilization process and avoid burning or damage to equipment. Only materials that are autoclavable should be placed inside the pressure chamber in order to avoid malfunction. A proper autoclave maintenance program and autoclave calibration are essential to keep the machine operating properly.
Operators must wear protective equipment while the loading process and when unloading. Watch for the sound of the sound of the whistle (pressure released) or for pressure to return to normal when opening the door. Avoid opening or cooling too quickly to avoid steam burns and biohazard control issues. The use of a sterilization log allows you to track every cycle to help validate the autoclave. These precautions ensure the safety of workers, protect instruments, and guarantee instrument sterilization and secure disposal of waste from microbiology labs as well as healthcare environments.
Be Precautious While Using Autoclaves
Utilizing an autoclave should be done with strict autoclave procedures to ensure laboratory security. Always inspect the gauge for pressure and the safety valve prior to starting the autoclave process. Only materials that can be autoclaved are allowed inside the sterilization chamber in order to avoid destruction. Making sure that the steam sterilizer is used correctly and following the autoclave procedure step by step can prevent accidents and assures sterility.
Wearing protective gear is essential for operators and be careful not to open the pressure chamber until the sound of a whistle (pressure release) sound. A careful monitoring of the sterilization temperature and pressure monitoring will ensure the safety of steam production. This prevents burns, limit biohazards and help ensure efficient thermal sterilization to kill microbial infections within labs and hospitals.
Calibration and Performance Qualification Testing of Autoclaves
Regular calibration of the autoclave and performance testing are essential for a precise steam sterilization. Testing will ensure that the pressure cooker type (also known as gravity displacement) is able to maintain the proper sterilization pressure and temperature. This confirms that the autoclave’s is working correctly in killing heat resistant microorganisms.
Utilizing indicator for sterilization, the spore tests on the autoclave, and sterilization record sheet, you can track and confirm the autoclave’s validation. A properly calibrated autoclave reduces contamination risk and facilitates effective sanitation of the instrument and waste sterilization. This will ensure a clean environment for healthcare sterilization and control of infections in Pakistan’s microbiology laboratories.
Purchase Considerations for Laboratory Autoclaves

Selecting the correct autoclave in microbiology will depend on many aspects including sterilization temperature, sterilization pressure and the type of autoclave used, like gravity displacement autoclaves or pressure cooker autoclave. The dimensions of your sterilization chamber must be able to accommodate the equipment you use in your lab and allow for proper steam flow for efficient thermal sterilization.
Also, be sure to look for important safety devices like a the safety valve, pressure gauge as well as whistle (pressure release) to ensure the safety of your autoclave. Correct calibration of the autoclave and monitoring of temperature ensure sterility and aid in the control of infection. The reliability of steam generation as well as a powerful vacuum pump enhance the autoclave process step by stage and guard against contamination by microbial.
Key Points Before Buying an Autoclave
When buying an autoclave for your laboratory be sure to consider the autoclave’s operation, the sterilization process and pressure for sterilization. Select the correct type of autoclave that you can use, for example, an autoclave with a pressure cooker or a gravity displacement autoclave depending on the sterilization requirements of your lab. Make sure the size of the sterilization chamber to match your lab equipment and make sure that it can support the use of moist heat for efficient removal of microbes.
Be aware of the calibration of your autoclave Pressure monitoring, calibration, and safety features of autoclaves such as the safety valves as well as pressure gauges. They can help maintain sterility and minimize the risk of biohazards being controlled. A reliable steam generator and a vacuum pump functions improve the penetration of steam and guarantee the proper sterilization of instruments for healthcare as well as research.
Interested in Learning More About Sterilization Equipment? Capasee Electro Medical Engineering Can Help
Capasee Electro Medical Engineering offers an array of high tech steam sterilizers and autoclaves specifically designed for sterilization in healthcare and safety in the laboratory. The products they offer include autoclaves that are suitable for sterilization of medical waste and sterilization of culture media and disinfection of instruments. They concentrate on a reliable autoclave procedures and validation of autoclaves to comply with international biosafety standards.
Their knowledgeable team assists customers in Pakistan by providing detailed advice regarding autoclave maintenance as well as autoclave calibration and monitoring of temperature. Capasee makes sure that users are aware of the what is the best practice for autoclaving with sterilization indicators as well as the spore test autoclave to ensure effective prevention of infection. Working with them ensures the safety of sterile, safe environment vital for hospital and lab work.
FAQ’s
What is the principle and purpose of autoclave?
Autoclave utilizes high pressure steam that kills microbes and ensure total sterilization of laboratory equipment and waste.
What is autoclave temperature?
The most common Autoclave’s temperature should be 121°C that effectively kills spores and bacteria.
Why autoclave at 121 C?
At 121°C, the steam sterilizer kills microbes that resist heat without harming instruments.
Why is autoclave done for 15 minutes?
A 15 minute timer at 121°C will ensure the destruction of spores and ensures sterility during the sterilization process.
What is the protocol for autoclave?
The process involves loading objects as well as setting temperatures and pressures, running the autoclave cycle, and finally safely unloading them after cooling.
Conclusion
The autoclave in microbiology plays crucially in ensuring the sterility of the environment making use of steam under pressure to ensure efficient microbial elimination. The steam sterilizer is a safe sterilization of lab equipment as well as culture media and medical waste. The correct use, calibration, and maintenance of the autoclave is vital to control infection and biosafety within laboratories. Knowing the procedure for autoclaving and following the best practices in autoclaving can help avoid contamination and ensure the reliability of scientific research which makes the autoclave a must in microbiology labs throughout Pakistan.